

Doctor Chamber
Apollo Gleneagles Cancer Hospital
58, Kanal Circular Road, Kadapara, kolkata 700054
Timing
Apollo Gleneagles Cancer Hospital
9:00 AM- 05:00 PM (Monday to Saturday)
Quick Contact
+918777427312
mesh.vicky@gmail.com
About Doctor
Dr Animesh Saha is a renowned Clinical Oncologist with excellent academic career and vast experience. He is currently working in Apollo Gleneagles Cancer Hospital, Kolkata as a Consultant Clinical Oncologist. Lately, He was working as a Consultant Clinical Oncologist (Sub specialty- Lung and Hepatobiliary cancers) in Leeds Cancer Centre, UK since November 2018. Prior to that, He was doing an International training fellowship in Clinical Oncology in the same Institute in UK from March 2017. Prior to that, He did his fellowship in Clinical Oncology from Tata Medical Centre, Kolkata from June 2013 to January 2017. He passed FRCR clinical Oncology exam in April 2018. He completed my MD Radiotherapy (From IPGME&R and SSKM hospital, Kolkata) in 2013 and DNB in 2014 in Radiation Oncology. He passed MBBS from R.G.Kar Medical College & Hospital, Kolkata back in 2008. He has keen interest in Lung, GI, Head & neck cancers, urological cancer and adult CNS tumours. He is practicing both Radiotherapy as well as systemic therapy for these sub sites. He has keen in interest in clinical research and He would be quite keen to set up collaborative intra-departmental research. He would also like to develop collaborative research with other centres in India as well as UK.
Services
Feedback
Caring attitude
Dr. Saha is very efficient Oncologist with caring attitude towards patients.
Subir Das
Durgapur
Very Good Treatment
Hi, everyone Dr. Animesh Saha is very good doctor, he has good expertise in oncologist.
Riya Dey
Salt Lake
Types of Cancer
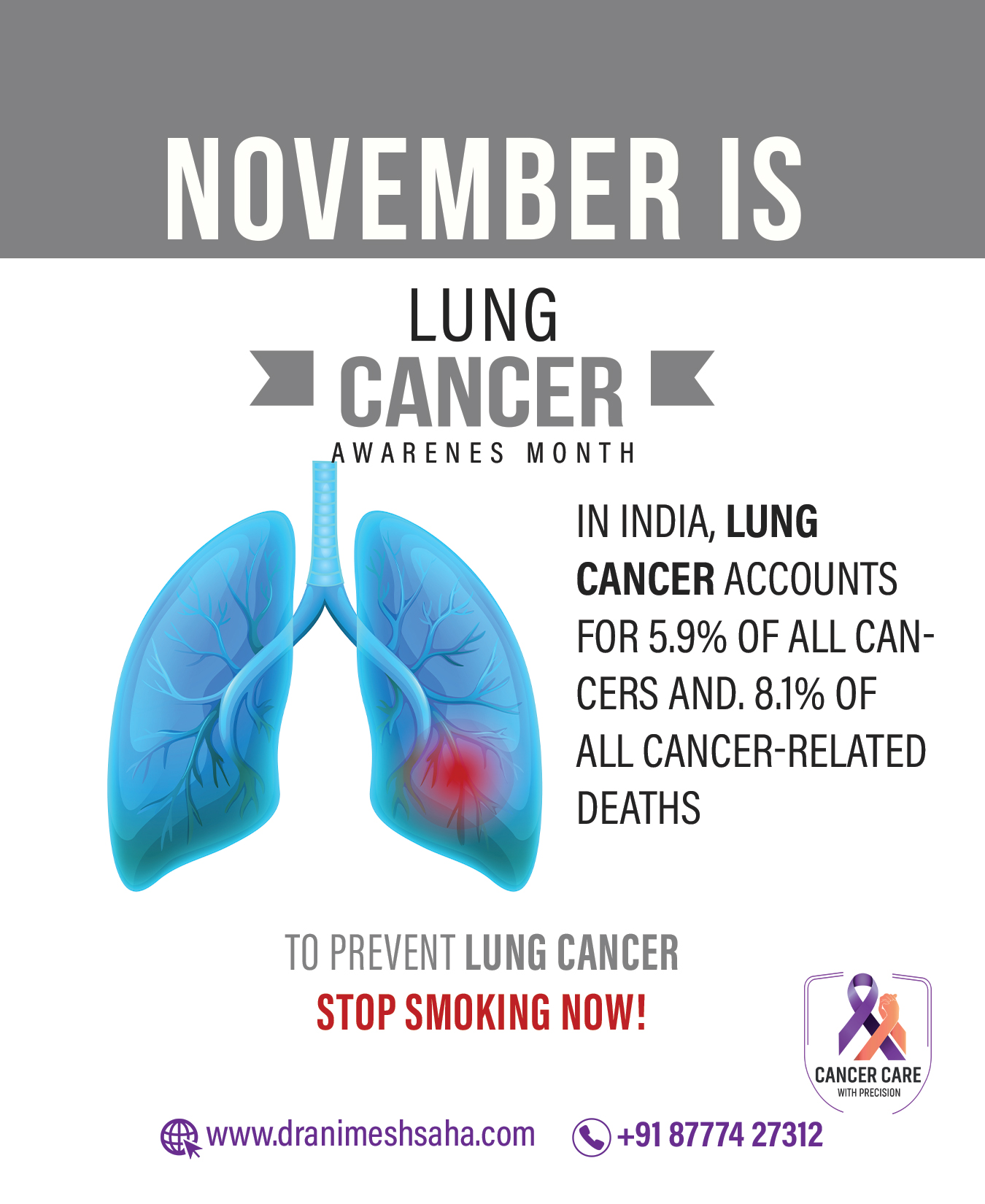
- Lung Cancer
- Head & Neck Cancer
- Brain Tumour
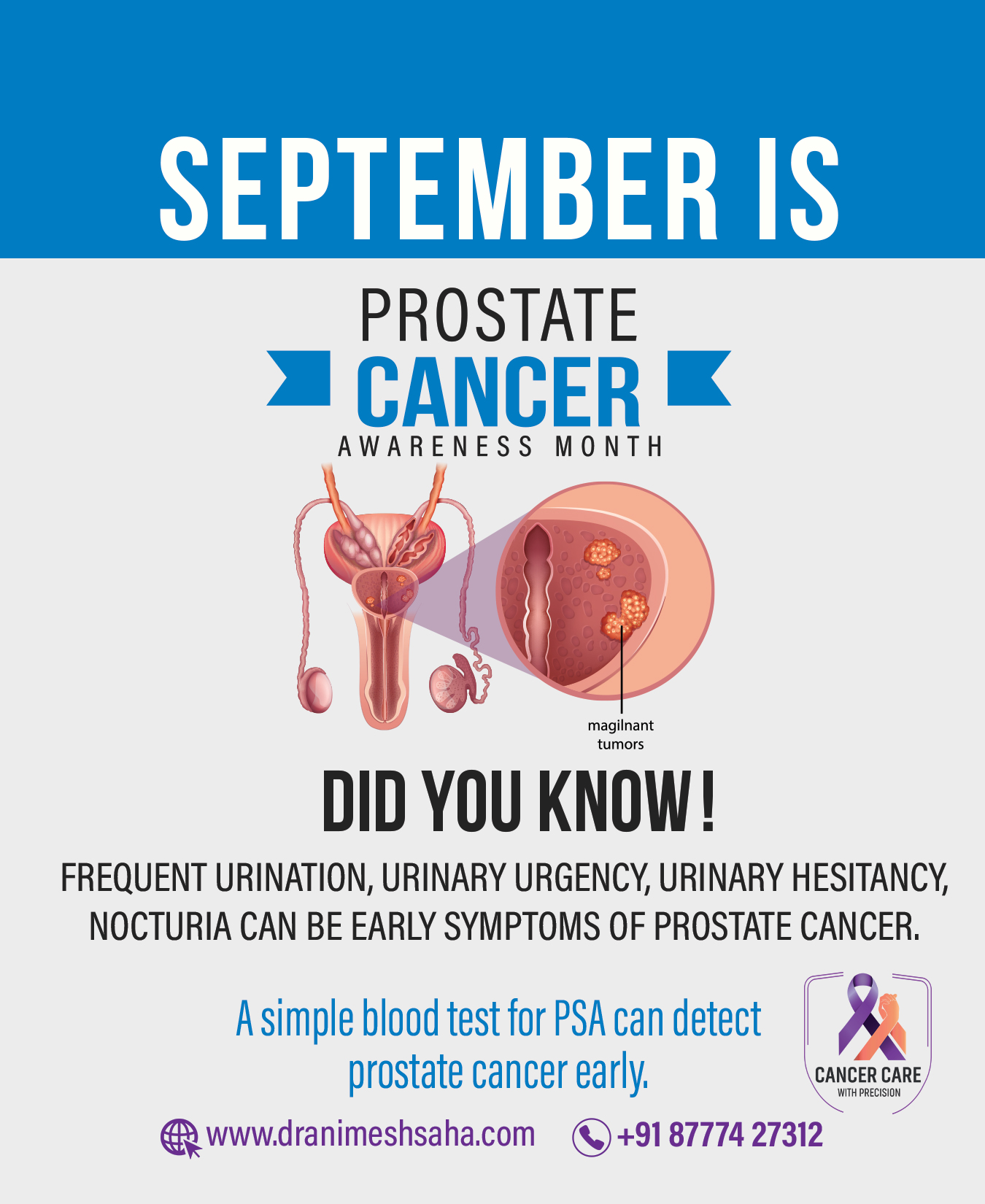
- Prostate Cancer
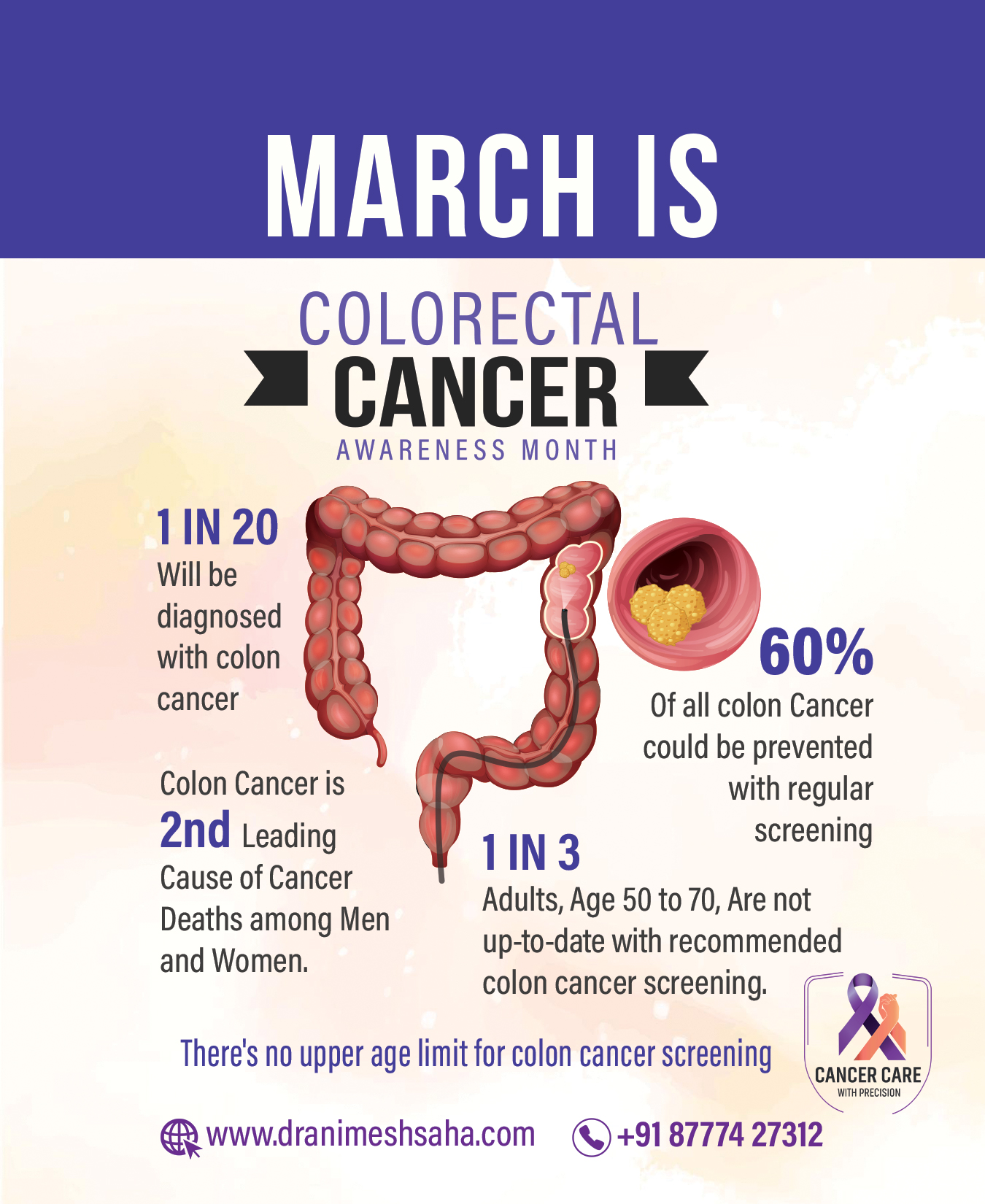
- Colorectal Cancer
- Oesophageal Cancer
- Pancreas Cancer
- Liver Cancer

Lung cancer, also known as lung carcinoma, is a malignant lung tumor characterized by uncontrolled cell growth in tissues of the lung. Lung cancer is now the most common cause of death from cancer. The two main types are small-cell lung carcinoma (SCLC) and non-small-cell lung carcinoma (NSCLC). The most common symptoms are coughing (including coughing up blood), weight loss, shortness of breath, and chest pains. About 90% lung cancer are caused by smoking. Lung cancer may be seen on chest radiographs, computed tomography (CT) scans and PET-CT scan. The diagnosis is confirmed by biopsy which is usually performed by bronchoscopy or CT-guidance. Treatment and long-term outcomes depend on the type of cancer, the stage (degree of spread), and the person’s overall health. Common treatments include surgery, chemotherapy, Immunotherapy and radiotherapy.
 Head and neck cancer is a group of cancers that starts in the mouth, nose, throat, larynx, sinuses, or salivary glands. Symptoms for head and neck cancer may include a lump or sore that does not heal, a sore throat that does not go away, trouble swallowing, or a change in the voice. There may also be unusual bleeding, facial swelling, or trouble breathing. About 75% of head and neck cancer is caused by the use of alcohol or tobacco. Other risk factors include betel quid, certain types of human papillomavirus, and Epstein-Barr virus. About 90% of head and neck cancers are squamous cell cancers. The diagnosis is confirmed by tissue biopsy. The degree of spread may be determined by medical imaging (CT scan, MRI or PET-CT scan). Head and neck cancer often is curable if it is diagnosed early; however, outcomes are typically poor if it is diagnosed late. Treatment may include a combination of surgery, radiation therapy, chemotherapy, Targeted therapy and Immunotherapy.
Head and neck cancer is a group of cancers that starts in the mouth, nose, throat, larynx, sinuses, or salivary glands. Symptoms for head and neck cancer may include a lump or sore that does not heal, a sore throat that does not go away, trouble swallowing, or a change in the voice. There may also be unusual bleeding, facial swelling, or trouble breathing. About 75% of head and neck cancer is caused by the use of alcohol or tobacco. Other risk factors include betel quid, certain types of human papillomavirus, and Epstein-Barr virus. About 90% of head and neck cancers are squamous cell cancers. The diagnosis is confirmed by tissue biopsy. The degree of spread may be determined by medical imaging (CT scan, MRI or PET-CT scan). Head and neck cancer often is curable if it is diagnosed early; however, outcomes are typically poor if it is diagnosed late. Treatment may include a combination of surgery, radiation therapy, chemotherapy, Targeted therapy and Immunotherapy.
 A brain tumour occurs when abnormal cells form within the brain. There are two main types of tumors: cancerous (malignant) tumors and benign (non-cancerous) tumors. Cancerous tumors can be divided into primary tumors, which start within the brain, and secondary tumors, which have spread from elsewhere, known as brain metastasis tumors. The symptoms may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking or with sensations. As the disease progresses, unconsciousness may occur.The cause of most brain tumors is unknown. Uncommon risk factors include exposure to vinyl chloride, Epstein–Barr virus, ionizing radiation, and inherited syndromes such as neurofibromatosis, tuberous sclerosis, and von Hippel-Lindau Disease. Studies on mobile phone exposure have not shown a clear risk. The most common types of primary tumors in adults are meningiomas (usually benign) and astrocytomas such as glioblastomas. In children, the most common type is a malignant medulloblastoma. Diagnosis is usually by medical examination along with computed tomography (CT) or magnetic resonance imaging (MRI). The result is then often confirmed by a biopsy. Based on the findings, the tumors are divided into different grades of severity. Treatment may include some combination of surgery, radiation therapy and chemotherapy. if seizures occur, anticonvulsant medication may be needed. Secondary, or metastatic, brain tumors are about four times more common than primary brain tumors, with about half of metastases coming from lung cancer.
A brain tumour occurs when abnormal cells form within the brain. There are two main types of tumors: cancerous (malignant) tumors and benign (non-cancerous) tumors. Cancerous tumors can be divided into primary tumors, which start within the brain, and secondary tumors, which have spread from elsewhere, known as brain metastasis tumors. The symptoms may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking or with sensations. As the disease progresses, unconsciousness may occur.The cause of most brain tumors is unknown. Uncommon risk factors include exposure to vinyl chloride, Epstein–Barr virus, ionizing radiation, and inherited syndromes such as neurofibromatosis, tuberous sclerosis, and von Hippel-Lindau Disease. Studies on mobile phone exposure have not shown a clear risk. The most common types of primary tumors in adults are meningiomas (usually benign) and astrocytomas such as glioblastomas. In children, the most common type is a malignant medulloblastoma. Diagnosis is usually by medical examination along with computed tomography (CT) or magnetic resonance imaging (MRI). The result is then often confirmed by a biopsy. Based on the findings, the tumors are divided into different grades of severity. Treatment may include some combination of surgery, radiation therapy and chemotherapy. if seizures occur, anticonvulsant medication may be needed. Secondary, or metastatic, brain tumors are about four times more common than primary brain tumors, with about half of metastases coming from lung cancer.
 Prostate cancer is the development of cancer in the prostate, a gland in the male reproductive system. Most prostate cancers are slow growing; however, some grow relatively quickly.The cancer cells may spread from the prostate to other areas of the body, particularly the bones and lymph nodes. Symptoms of prostate cancer includes difficulty urinating, blood in the urine or pain in the pelvis, back, or when urinating. About 99% of cases occur in males over the age of 50. Prostate cancer is diagnosed by biopsy . Medical imaging (CT scan, MRI scan, Bone scan or PSMA PET-CT scan) may then be done to determine if the cancer has spread to other parts of the body. Serum PSA is the tumour marker for prostate cancer. Prostate cancer screening is controversial. Prostate-specific antigen (PSA) testing increases cancer detection, but it is controversial regarding whether it improves outcomes. Informed decision making is recommended when it comes to screening among those 55 to 69 years old. Many cases are managed with active surveillance or watchful waiting.[2] Other treatments may include a combination of surgery, radiation therapy, hormone therapy or chemotherapy.[2] When it only occurs inside the prostate, it may be curable.[1] In those in whom the disease has spread to the bones, pain medications, bisphosphonates and targeted therapy, among others, may be useful.
Prostate cancer is the development of cancer in the prostate, a gland in the male reproductive system. Most prostate cancers are slow growing; however, some grow relatively quickly.The cancer cells may spread from the prostate to other areas of the body, particularly the bones and lymph nodes. Symptoms of prostate cancer includes difficulty urinating, blood in the urine or pain in the pelvis, back, or when urinating. About 99% of cases occur in males over the age of 50. Prostate cancer is diagnosed by biopsy . Medical imaging (CT scan, MRI scan, Bone scan or PSMA PET-CT scan) may then be done to determine if the cancer has spread to other parts of the body. Serum PSA is the tumour marker for prostate cancer. Prostate cancer screening is controversial. Prostate-specific antigen (PSA) testing increases cancer detection, but it is controversial regarding whether it improves outcomes. Informed decision making is recommended when it comes to screening among those 55 to 69 years old. Many cases are managed with active surveillance or watchful waiting.[2] Other treatments may include a combination of surgery, radiation therapy, hormone therapy or chemotherapy.[2] When it only occurs inside the prostate, it may be curable.[1] In those in whom the disease has spread to the bones, pain medications, bisphosphonates and targeted therapy, among others, may be useful.
 Colorectal cancer (CRC), also known as bowel cancer, colon cancer, or rectal cancer, is the development of cancer from the colon or rectum (parts of the large intestine). Signs and symptoms may include blood in the stool, a change in bowel movements, weight loss, and feeling tired all the time.Most colorectal cancers are due to old age and lifestyle factors, with only a small number of cases due to underlying genetic disorders.Other risk factors include diet, obesity, smoking, and lack of physical activity. Dietary factors that increase the risk include red meat, processed meat, and alcohol. Another risk factor is inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis. Some of the inherited genetic disorders that can cause colorectal cancer include familial adenomatous polyposis and hereditary non-polyposis colon cancer. Bowel cancer may be diagnosed by obtaining a sample of the colon during a sigmoidoscopy or colonoscopy. This is then followed by medical imaging ( CT scan, MRI scan or PET-CT scan) to determine if the disease has spread. Treatments used for colorectal cancer may include some combination of surgery, radiation therapy, chemotherapy and targeted therapy.Cancers that are confined within the wall of the colon may be curable with surgery, while cancer that has spread widely is usually not curable, with management being directed towards improving quality of life and symptoms.
Colorectal cancer (CRC), also known as bowel cancer, colon cancer, or rectal cancer, is the development of cancer from the colon or rectum (parts of the large intestine). Signs and symptoms may include blood in the stool, a change in bowel movements, weight loss, and feeling tired all the time.Most colorectal cancers are due to old age and lifestyle factors, with only a small number of cases due to underlying genetic disorders.Other risk factors include diet, obesity, smoking, and lack of physical activity. Dietary factors that increase the risk include red meat, processed meat, and alcohol. Another risk factor is inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis. Some of the inherited genetic disorders that can cause colorectal cancer include familial adenomatous polyposis and hereditary non-polyposis colon cancer. Bowel cancer may be diagnosed by obtaining a sample of the colon during a sigmoidoscopy or colonoscopy. This is then followed by medical imaging ( CT scan, MRI scan or PET-CT scan) to determine if the disease has spread. Treatments used for colorectal cancer may include some combination of surgery, radiation therapy, chemotherapy and targeted therapy.Cancers that are confined within the wall of the colon may be curable with surgery, while cancer that has spread widely is usually not curable, with management being directed towards improving quality of life and symptoms.
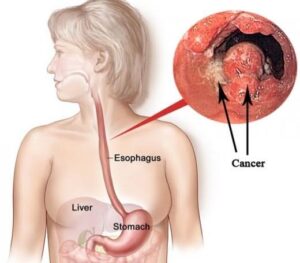 Esophageal cancer is cancer arising from the esophagus—the food pipe that runs between the throat and the stomach.Symptoms often include difficulty in swallowing and weight loss. Other symptoms may include pain when swallowing, a hoarse voice, enlarged lymph nodes (“glands”) around the collarbone, a dry cough, and possibly coughing up or vomiting blood.The two main sub-types of the disease are esophageal squamous-cell carcinoma which is more common in the developing world, and esophageal adenocarcinoma , which is more common in the developed world. Causes of the squamous-cell type include tobacco, alcohol, very hot drinks, poor diet, and chewing betel nut. The most common causes of the adenocarcinoma type are smoking tobacco, obesity, and acid reflux.The disease is diagnosed by biopsy done by an endoscope (a fiberoptic camera). CT Scan or PET-CT scan usually done to stage the cancer. Treatment is based on the cancer’s stage and location, together with the person’s general condition and individual preferences. Small-localized squamous-cell cancers may be treated with surgery alone with the hope of a cure. In most other cases, chemotherapy with or without radiation therapy is used along with surgery. Larger tumors may have their growth slowed with chemotherapy and radiation therapy. In the presence of extensive disease or if the affected person is not fit enough to undergo surgery, palliative care is often recommended. As of 2018, esophageal cancer was the eighth-most common cancer globally with 572,000 new cases during the year.
Esophageal cancer is cancer arising from the esophagus—the food pipe that runs between the throat and the stomach.Symptoms often include difficulty in swallowing and weight loss. Other symptoms may include pain when swallowing, a hoarse voice, enlarged lymph nodes (“glands”) around the collarbone, a dry cough, and possibly coughing up or vomiting blood.The two main sub-types of the disease are esophageal squamous-cell carcinoma which is more common in the developing world, and esophageal adenocarcinoma , which is more common in the developed world. Causes of the squamous-cell type include tobacco, alcohol, very hot drinks, poor diet, and chewing betel nut. The most common causes of the adenocarcinoma type are smoking tobacco, obesity, and acid reflux.The disease is diagnosed by biopsy done by an endoscope (a fiberoptic camera). CT Scan or PET-CT scan usually done to stage the cancer. Treatment is based on the cancer’s stage and location, together with the person’s general condition and individual preferences. Small-localized squamous-cell cancers may be treated with surgery alone with the hope of a cure. In most other cases, chemotherapy with or without radiation therapy is used along with surgery. Larger tumors may have their growth slowed with chemotherapy and radiation therapy. In the presence of extensive disease or if the affected person is not fit enough to undergo surgery, palliative care is often recommended. As of 2018, esophageal cancer was the eighth-most common cancer globally with 572,000 new cases during the year.
 Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. There are a number of types of pancreatic cancer. The most common, pancreatic adenocarcinoma, accounts for about 85% of cases, and the term “pancreatic cancer” is sometimes used to refer only to that type. These adenocarcinomas start within the part of the pancreas which makes digestive enzymes. One to two percent of cases of pancreatic cancer are neuroendocrine tumors, which arise from the hormone-producing cells of the pancreas. These are generally less aggressive than pancreatic adenocarcinoma. Signs and symptoms of the most-common form of pancreatic cancer may include yellow skin, abdominal or back pain, unexplained weight loss, light-colored stools, dark urine, and loss of appetite. Risk factors for pancreatic cancer include tobacco smoking, obesity, diabetes, and certain rare genetic conditions. Pancreatic cancer is usually diagnosed by a combination of medical imaging techniques such as ultrasound or computed tomography, MRCP, blood tests, and examination of tissue samples (biopsy). The disease is divided into stages, from early (stage I) to late (stage IV). Pancreatic cancer can be treated with surgery, radiotherapy, chemotherapy, palliative care, or a combination of these.Treatment options are partly based on the cancer stage. Surgery is the only treatment that can cure pancreatic adenocarcinoma, and may also be done to improve quality of life without the potential for cure.
Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. There are a number of types of pancreatic cancer. The most common, pancreatic adenocarcinoma, accounts for about 85% of cases, and the term “pancreatic cancer” is sometimes used to refer only to that type. These adenocarcinomas start within the part of the pancreas which makes digestive enzymes. One to two percent of cases of pancreatic cancer are neuroendocrine tumors, which arise from the hormone-producing cells of the pancreas. These are generally less aggressive than pancreatic adenocarcinoma. Signs and symptoms of the most-common form of pancreatic cancer may include yellow skin, abdominal or back pain, unexplained weight loss, light-colored stools, dark urine, and loss of appetite. Risk factors for pancreatic cancer include tobacco smoking, obesity, diabetes, and certain rare genetic conditions. Pancreatic cancer is usually diagnosed by a combination of medical imaging techniques such as ultrasound or computed tomography, MRCP, blood tests, and examination of tissue samples (biopsy). The disease is divided into stages, from early (stage I) to late (stage IV). Pancreatic cancer can be treated with surgery, radiotherapy, chemotherapy, palliative care, or a combination of these.Treatment options are partly based on the cancer stage. Surgery is the only treatment that can cure pancreatic adenocarcinoma, and may also be done to improve quality of life without the potential for cure.
 Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. There are a number of types of pancreatic cancer. The most common, pancreatic adenocarcinoma, accounts for about 85% of cases, and the term “pancreatic cancer” is sometimes used to refer only to that type. These adenocarcinomas start within the part of the pancreas which makes digestive enzymes. One to two percent of cases of pancreatic cancer are neuroendocrine tumors, which arise from the hormone-producing cells of the pancreas. These are generally less aggressive than pancreatic adenocarcinoma. Signs and symptoms of the most-common form of pancreatic cancer may include yellow skin, abdominal or back pain, unexplained weight loss, light-colored stools, dark urine, and loss of appetite. Risk factors for pancreatic cancer include tobacco smoking, obesity, diabetes, and certain rare genetic conditions. Pancreatic cancer is usually diagnosed by a combination of medical imaging techniques such as ultrasound or computed tomography, MRCP, blood tests, and examination of tissue samples (biopsy). The disease is divided into stages, from early (stage I) to late (stage IV). Pancreatic cancer can be treated with surgery, radiotherapy, chemotherapy, palliative care, or a combination of these.Treatment options are partly based on the cancer stage. Surgery is the only treatment that can cure pancreatic adenocarcinoma, and may also be done to improve quality of life without the potential for cure.
Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. There are a number of types of pancreatic cancer. The most common, pancreatic adenocarcinoma, accounts for about 85% of cases, and the term “pancreatic cancer” is sometimes used to refer only to that type. These adenocarcinomas start within the part of the pancreas which makes digestive enzymes. One to two percent of cases of pancreatic cancer are neuroendocrine tumors, which arise from the hormone-producing cells of the pancreas. These are generally less aggressive than pancreatic adenocarcinoma. Signs and symptoms of the most-common form of pancreatic cancer may include yellow skin, abdominal or back pain, unexplained weight loss, light-colored stools, dark urine, and loss of appetite. Risk factors for pancreatic cancer include tobacco smoking, obesity, diabetes, and certain rare genetic conditions. Pancreatic cancer is usually diagnosed by a combination of medical imaging techniques such as ultrasound or computed tomography, MRCP, blood tests, and examination of tissue samples (biopsy). The disease is divided into stages, from early (stage I) to late (stage IV). Pancreatic cancer can be treated with surgery, radiotherapy, chemotherapy, palliative care, or a combination of these.Treatment options are partly based on the cancer stage. Surgery is the only treatment that can cure pancreatic adenocarcinoma, and may also be done to improve quality of life without the potential for cure.
Cancer Awareness Months






Patient's Feedback
Trustindex verifies that the original source of the review is Google. My father Shri Dulal Krishna Dey was under the treatment of Dr. Animesh Saha for a prolonged time of nearly six weeks in two phases. I found Dr. Saha not only a good doctor but a nice gentleman with a grounded and disciplined approach to resolve the problem which is now a days a very rare quality available among most of young doctors. As an Oncologist his approach to diagnose the root cause and treatment was very well planned and he was always transparent regarding his treatment without giving any false hope to me ,being realistic of the outcome all the time. He arranged a medical board to decide the way forward for my father’s treatment which was a pleasant surprise for me as I never expected such things in India. I do not know how long my father will survive post his radiation therapy by Dr. Saha, but that won’t affect my appreciation and regard for him which he earned at his own right at such a young age. Hope he will keep his similar outstanding humancentric treatment approach in years to come and his future success won’t change him as a human being. Wish him all the best.Trustindex verifies that the original source of the review is Google. Not only 5stars. May be 5000 stars are less to appreciate him.. Incredible joy to share my experience. Excellent behavior and heart touching journey with splendid outcome..Trustindex verifies that the original source of the review is Google. Dr.saha is one of the best oncologist in Kolkata..my father was suffering from lung cancer and he is 69 year old.but now my father is absolutely fine and curred by dr.saha's treatment. Dr.saha is not only a good doctor also a very good human being..he help us like a angel .. I personally believe he is best oncologist in eastern India.. Dr.saha is Angel for my family.. Thank you so much Dr.Animesh saha(sir).Trustindex verifies that the original source of the review is Google. Depth of field is a term I borrow from photography. It applies so aptly to Dr. Saha. Add to that, a mighty heart. A rare combination indeed.Trustindex verifies that the original source of the review is Google. Excellent experience! I highly recommend Dr Saha and wish that anybody who has to go through such a trying time has smooth & successful journey!Trustindex verifies that the original source of the review is Google. We will be grateful to Dr Saha for the care we received for my patient. He has taken great effort to explain us about the patient's condition everytime. His calm, humble and careful attitude towards patients is praiseworthy. We wish Dr Saha all the best for his future career..... Keep doing good work...
Advanced Technology
Dr Saha uses conventional as well as latest technologies in radiation oncology and medical oncology to treat cancer.
Evidence Based Medicine
Evidence based medicine (EBM) is the conscientious, explicit, judicious and reasonable use of modern, best evidence in making decisions about the care of cancer patients.
Comprehensive Cancer Care
Comprehensive and multidisciplinary care – means that specialists from different medical disciplines collaborate to plan, evaluate and deliver cancer treatment.